Weight loss surgery
Weight loss surgery is also known as bariatric surgery. It aims to reduce weight and improve medical conditions which are associated with obesity.1

Who qualifies for weight loss surgery?
Your doctor may consider you for bariatric surgery if these conditions apply to you:2
- Your BMI is over 40.
- Your BMI is over 35 and you have a comorbidity that may improve with weight loss.
- Your BMI is over 30 and you have uncontrolled type 2 diabetes and at increased cardiovascular risk.
You must show that you’re committed to making lifestyle changes and you need to understand the risks of surgery and agree to followup care.
Disclaimer: Consult your doctor for weight management and get help to work out what weight loss plan is best for you.
How does bariatric surgery work?
Weight loss surgery works by increasing the feeling of fullness after you eat.3 4
Most weight loss surgeries in New Zealand are performed laparoscopically. That means they’re key-hole surgery.5
When you have key-hole surgery, you usually spend less time in hospital, have fewer complications and it takes less time to make a full recovery compared to open surgery.6 7 8
The average length of stay in hospital for patients after bariatric surgery is between 1.9 and 2.8 days, depending on which procedure you have done.9
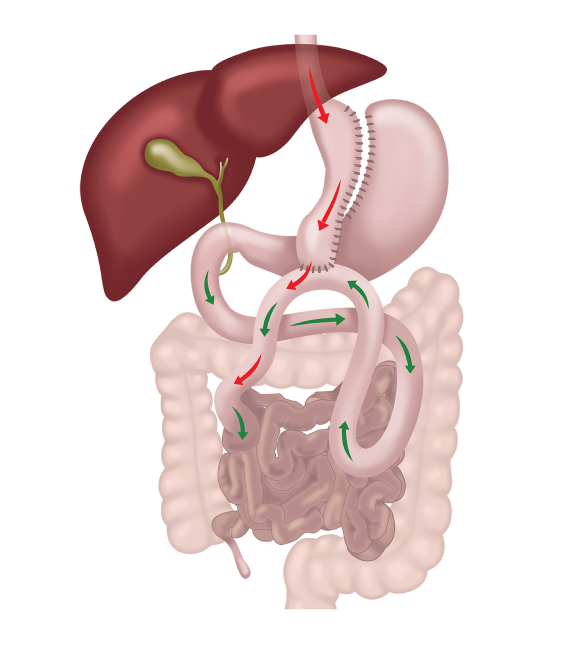
Types of bariatric surgeries
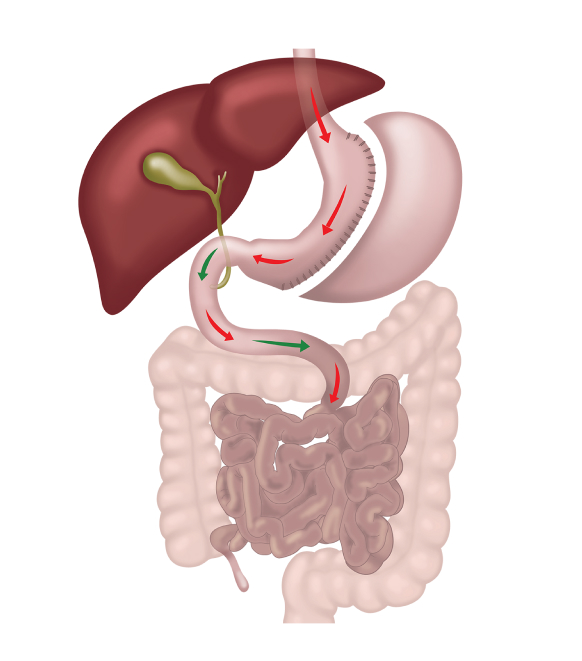
Roux-en-y gastric bypass surgery
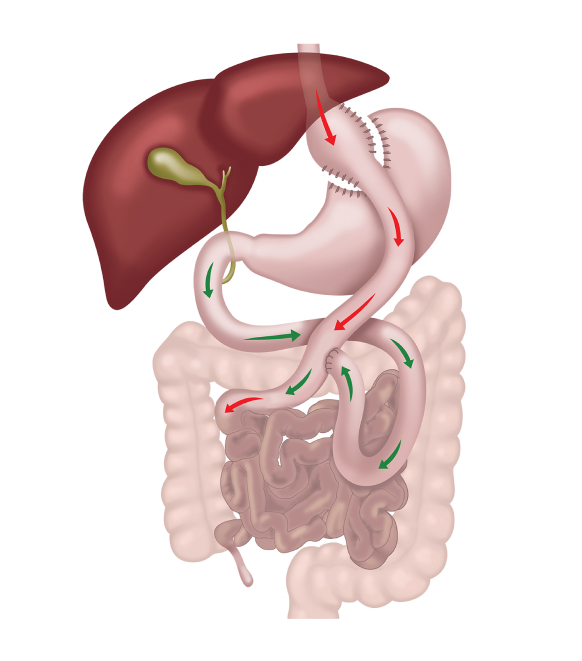
One anastomosis gastric bypass surgery
How well does bariatric surgery work for weight loss?
Of all the weight loss strategies, studies have shown that surgery leads to the greatest and most sustained weight loss for people with obesity.2 13
After three years, the average weight loss is 24%. By 5 years, the average weight loss is 19%.10
There are other health advantages too. 31-77% of people with type 2 diabetes manage normal blood sugar without diabetes medication after weight loss surgery. 80% maintain good glycaemic control with reduced or no medication.14
Other reported improvements include:1 14 15 16
- Lower cardiovascular risk factors (stroke, high blood pressure, high cholesterol)
- Improved kidney function
- Reduced respiratory diseases such as asthma and sleep apnoea
- Less reflux disease
- A better quality of life
What are the risks of weight loss surgery?
Like any medical intervention, bariatric surgery has risks, including the risk of surgical failure, complications, even in rare cases, death.1 16
Of the over 70,000 patients in Australia and New Zealand who have had surgery since 2012, 0.8% had to have another operation to fix a problem. Less than 1% have been re-admitted to hospital with a complication.10
In 2018-19, the rates of adverse events ranged from 1.6% (sleeve gastrectomy) to 6.3% (roux-en-y gastric bypass surgery).10
What should you consider before thinking about weight loss surgery?
Bariatric surgery is not a quick fix. You need long term commitment to get the best outcomes.
You will need to make substantial lifestyle changes before your surgery. This might mean giving up smoking and most patients will need to use meal replacements for 2-4 weeks beforehand to increase safety of the surgery.1
After your weight loss surgery, you will have to follow a healthy lifestyle plan and you will need to take vitamin and mineral supplements for the rest of your life. It’s important that you work on your mental health and get help if you need it, as it will increase your chances of success.17
Obesity is a chronic and progressive disease and there is a high likelihood that you may regain some weight at some point. If you stay connected with your healthcare team, you can help minimise weight gain and live a healthy, active lifestyle.1